Men can also grow breasts. And no, it often has nothing to do with beer, as many might think. It’s a completely natural occurrence among men. Some can learn to cope with their gynecomastia, but at the end of the day, it can negatively affect their self-esteem. So, is it possible to somehow reduce the male breast?
In this article, together with Dr. Wendell Uguetto, we will talk about gynecomastia: what it is, what triggers it, and how to deal with it.
What Is Gynecomastia?
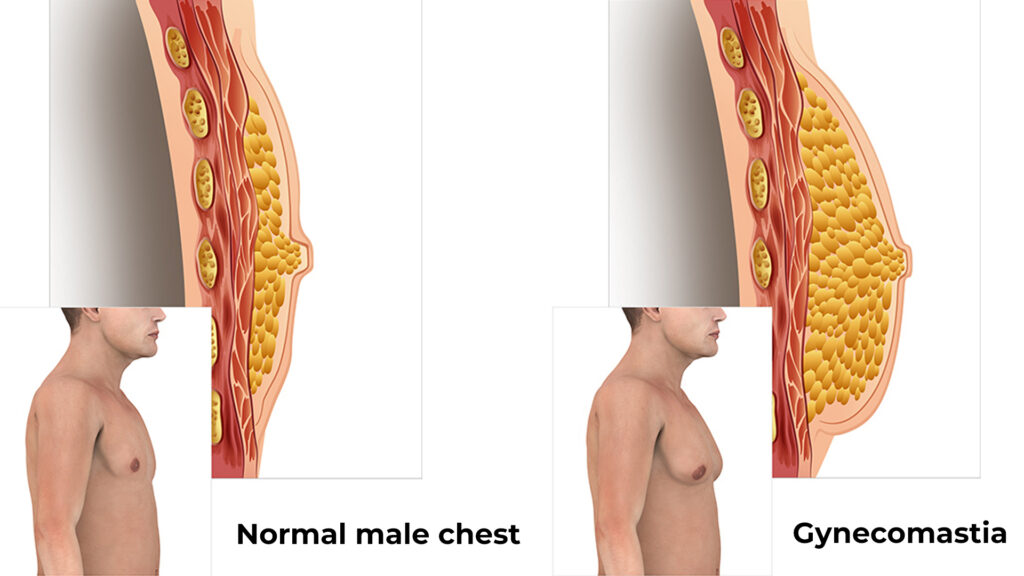
Gynecomastia is the abnormal enlargement of breast tissue in men, caused by hormonal disruption, leading to mammal gland changes. Not to be confused with pseudogynecomastia, which is simply fat.
As Dr. Uguetto explains, “Regardless of gender, humans are mammals, and all mammals, including humans, are born with a little mammary gland. In females, estrogen prompts breast growth during adolescence to prepare for lactation. Men, however, produce little to no estrogen, so substantial breast enlargement caused by excess estrogen is considered gynecomastia.”
Such a condition can happen to any man at any age, but it usually occurs in two cases: in adolescence, when puberty starts, and during andropauseAndropause, also known as 'male menopause', is a term that refers to a decrease in male hormone production, primarily testosterone, at age 55-60., when the production of testosterone naturally drops in the testicles, and estrogen increases proportionally, leading to gynecomastia.
Gynecomastia can lead to psychological distress and discomfort for men, potentially impacting their quality of life. It can also point out other hormonal issues, which we will discuss further. Additionally, men with gynecomastia have a slightly higher risk of developing breast cancer (about 1% of all gynecomastia cases) compared to men without the condition [5].
Types of Gynecomastia
Gynecomastia is categorized based on how severe the mammal gland is increased and by the presence of excess skin. Dr. Wendell Uguetto shared insights about each category. During patient assessment, they are classified into one of three grades: mild, moderate, and severe [2].
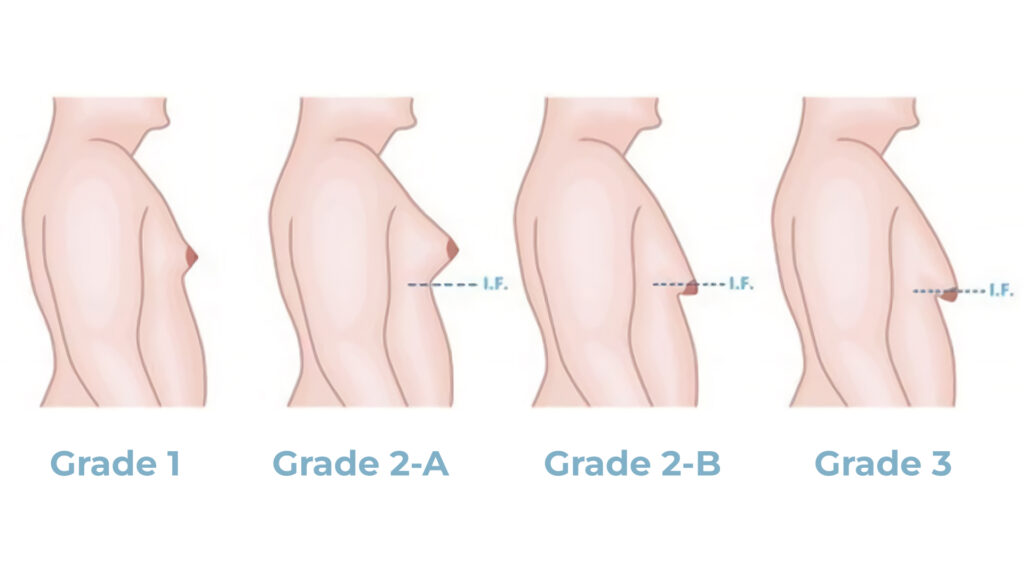
Grade I: Mild gynecomastia
Grade 1 is most commonly found mostly among children during puberty, signifying a small increase in breast tissue size. Even Dwayne Johnson (The Rock) had minor gynecomastia surgery!
In this case, the breast has a volume of fewer than 250 grams on one side without any noticeable skin sagging. This grade is identified by firm tissue localized around the nipple area.
Both children and adult men with small gynecomastia may complain of nipple protrusion, especially in hot weather when they become more noticeable through thin clothing, like white T-shirts. They might also feel embarrassed wearing tight-fitting clothing, such as dry-fit shirts, in the gym.
Grade II: Moderate gynecomastia
Grade II represents moderate gynecomastia and has two subtypes: 2-A and 2-B, with the breast volume ranging between 250 and 750 grams per side. Now, a breast with this grade becomes more visible through clothing, which leads to men adopting coping mechanisms like wearing thicker, darker clothing for camouflage despite any conditions, and hunching their shoulders inward.
Here’s what Dr. Uguetto commented on how gynecomastia affects posture: “Most of my patients come with rotated scapulae or arched shoulders. Even the most confident men can be affected by this on a subconscious level. They know about this flaw, they live with it, and they try to hide it, which results in musculoskeletal issues.”
The difference between 2-A and 2-B lies in the amount of excess skin. The 2-A grade is classified as less severe, with no excess skin present while grade 2-B shows its presence, which may cause the breast tissue to appear more pendulous (drooping) and jiggle during activities like running or jumping.
Grade III: Severe gynecomastia
This is the most severe form of gynecomastia. Patients with Grade III gynecomastia have much more excess skin along with enlarged breast tissue and areolas. Here, the breast tissue volume exceeds 750 grams on one side.
Compared to previous grades, this one causes discomfort and limitations during physical activities due to the breasts’ weight and movement. Even shopping becomes challenging, as many clothing sizes start to feel and look too wide in the waist and too tight in the chest area.
Regardless of the type of gynecomastia, young men can be bullied because of it and have major self-esteem issues. Dr. Uguetto noted that “Intuitively and unconsciously, they begin to hunch the shoulders and wear larger, darker clothes to disguise the flaw.”
What Causes Gynecomastia?

Contrary to popular belief, gynecomastia isn’t a recent phenomenon, but rather a natural occurrence in many adolescents [1]. According to Dr. Uguetto, up to 70% of boys going through puberty can develop some degree of gynecomastia.
“Gynecomastia has always been around, but it may seem more common now simply because awareness has increased. In the past, men might’ve experienced symptoms but didn’t know what caused them or were hesitant to seek help. With more widespread information, they can identify and address the condition with proper care.”
— Dr. Wendell Uguetto
Male breast growth can occur due to various factors. Dr. Wendell Uguetto pointed out three main gynecomastia causes: physiological, pathological, and medicinal. Let’s briefly introduce each of them.
Physiological Causes
The physiological causes of gynecomastia are divided into two types, both related to the development of the male and their hormones. As mentioned by Dr. Uguetto, “We call them physiological because they are natural hormonal changes.”
The most common type of physiological gynecomastia is adolescent gynecomastia, which occurs during puberty and is caused by erratic testosterone production. As the testes begin testosterone production, there can be temporary imbalances that lead to breast tissue development. However, this typically resolves on its own within a year or so.
“In most cases of pediatric gynecomastia, we do not resort to surgical intervention unless it critically affects the child’s health. In 90% of cases, gynecomastia goes away on its own when hormone production stabilizes. Alas, those who don’t have it go away have to live with it all their lives, and then they can think about surgery.”
— Dr. Wendell Uguetto
The second type of physiological cause, neonatal gynecomastia, is much rarer. Newborns can experience temporary breast enlargement due to residual maternal hormones passed through breast milk. “For a baby, it’s quite an unpleasant experience, they can feel pain and cry because of how this gynecomastia feels,” adds Dr. Uguetto. This type of gynecomastia regresses by itself within a few weeks after stopping breastfeeding.
Pathological Causes
Gynecomastia can also arise from underlying medical conditions known as pathological causes. We can name several medical conditions that can directly impact testosterone levels, leading to gynecomastia, including tumors, Klinefelter syndromeMen born with an extra X chromosome (XXY chromosomes instead of XY)., hypogonadismChronic low testosterone., and hyperthyroidismOveractive thyroid gland, resulting in a speed-up metabolism..
Dr. Uguetto notes that the tumor does not necessarily have to be in the testicles to cause hormonal disruption: “A tumor in the pituitary gland, located at the base of the brain, can produce hormones like prolactin, which can lead to a drop in testosterone levels in excessive amounts, and potentially cause gynecomastia.”
He also mentioned kidney tumors as another pathology: “Adrenal tumors, which are located on top of the kidneys, can produce an excess of cortisol, a hormone that can indirectly lower testosterone and contribute to gynecomastia.”
Among the not-so-obvious pathologies that can affect the development of gynecomastia are liver problems. “A failing liver loses its ability to break down estrogen effectively, leading to higher estrogen levels, which again, may cause gynecomastia,” emphasized Dr. Uguetto.
Medical Causes
Certain medications, especially those that can impact hormonal disbalance, can trigger gynecomastia as a side effect.
For example, it may be caused by medications for prostate, digestion, hair loss, blood pressure regulation, antidepressants, anticonvulsants, etc. Even Dr. Uguetto himself had to experience a similar side effect, but in his case, gynecomastia regressed three months after stopping the medication.
Gynecomastia can also occur due to long-term drug use (e.g. marijuana, heroin, or amphetamines), as well as unregulated or accidental use of female hormonal contraceptives by children [3].
Treatment for Gynecomastia
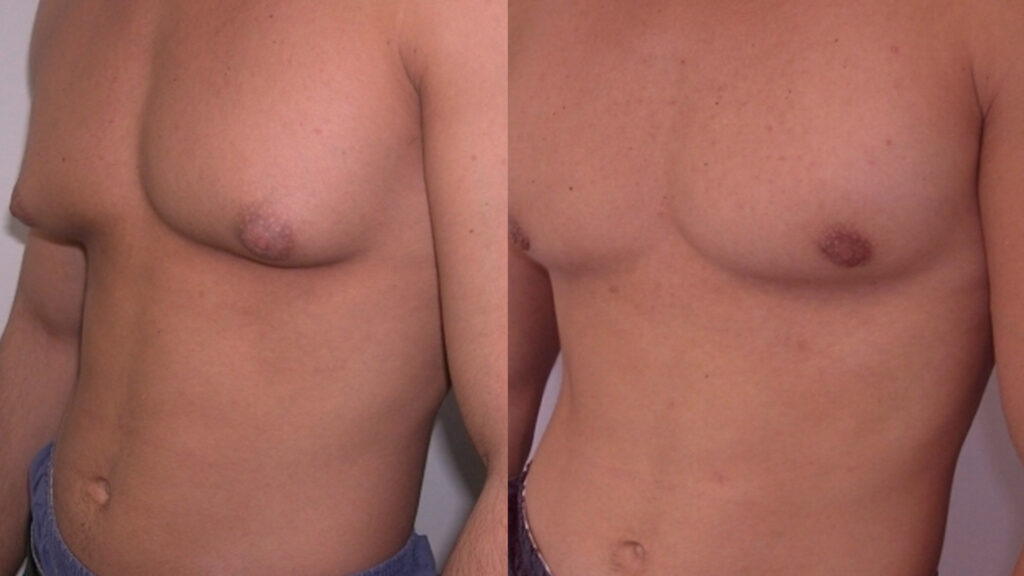
Gynecomastia surgery aims to reduce enlarged male breasts. Here, we will explain the different surgical techniques available, when the surgery treatment is necessary, and whether it’s suitable for children.
Taking Medication
For patients with gynecomastia less than a year and a half old, Dr. Uguetto favors a combination medication approach, which involves mammary gland hormone receptor blockers and aromatase inhibitors (e.g., anastrozole).
Medication is most effective for gynecomastia in its early stages (less than 1.5 years). After this timeframe, the tissue becomes fibrous and less responsive to medication, making surgery a more likely option.
Receptor blockers combined with anastrozole boast a success rate of up to 70% for treatable gynecomastia. However, Dr. Uguetto acknowledges the potential side effects of tamoxifenBreast cancer hormonal treatment., including depression, weight gain, and decreased libido, and limits its use to a maximum of 2–3 months due to its limited effectiveness (around 40%).
To conclude, from a general point of view, gynecomastia lasts less than a year and a half — medication is the way out. For more than a year and a half — surgery is a likely option.
Surgery Techniques
The most common approach to gynecomastia is the Webster’s technique [4]. “It involves liposuction first, followed by a side incision for further fat removal. Then, a half-moon incision around the areola allows removal of the glandular tissue,” defined Dr. Uguetto.
Webster’s technique avoids removing the skin, minimizing scarring, but it involves a risk of necrosis around the areola.
Dr. Uguetto also details his own surgery method, which minimizes the risk of necrosis, heals faster, and leaves invisible scarring:
“My technique utilizes a small incision on the chest side for initial liposuction. Then, a specialized tool with a light source is inserted through the same opening to remove the gland. This approach avoids any cuts around the areola.”
— Dr. Wendell Uguetto
Another benefit of Dr. Uguetto’s technique is that it downscales the risk of recurrence. “Recurrence can happen in up to 5% of Webster surgeries because some glandular tissue might remain,” says Dr. Uguetto. “By removing more tissue with a 3-millimeter safety zone below the areola, my technique boasts a much lower recurrence rate of 0.5%. And it looks better aesthetically.”
Pediatric Gynecomastia
As we mentioned earlier, gynecomastia most often occurs in adolescence and can go away on its own. In the case of neonatal gynecomastia, there is no need for surgical intervention, as in this case, it is enough to simply stop breastfeeding.
Generally speaking, Dr. Uguetto doesn’t recommend immediate surgical intervention for adolescents, unless, of course, the existing gynecomastia has a significant impact on their mental state. “When the gynecomastia is recent, we try to encourage the child to lose weight, do some physical activity, wait a while, disguise it, to see if gynecomastia disappears,” highlights Dr. Uguetto.
The wait for gynecomastia regression on its own lasts about 1.5 years since it cannot regress anymore after that. However, if the case is severe, and the child suffers greatly mentally from it, there is a possibility of surgical intervention even at the age of 12.
Contradictions & Complications
With surgery involvement, scarring is inevitable. However, since men are used to shirtless outfits, their gyno surgery scar can cause some social inconvenience. For example, when going to the beach. The size of the scar is often proportional to the amount of tissue removed.
In most cases, with experienced surgeons, the procedure is quick and safe, with hematoma and seroma possibly occurring only in 5-10% of cases. Most complications (also rare) are associated with necrosis and loss of sensation.
If gynecomastia can be treated without surgery, it is better to do so. According to this principle, age is the first contraindication. Regarding teenage gynecomastia, Dr. Uguetto prefers to wait and observe if it can resolve on its own with natural hormonal changes.
Similarly, Dr. Uguetto mentioned that he doesn’t resort to plastic surgery if the examination shows the problem lying in something else.
“I treat the cause first. So, if I have a patient with testicular cancer, I don’t treat the gynecomastia, I treat cancer. And if I have a patient with liver failure, I don’t treat gynecomastia, I treat liver failure. In these cases, you treat the disease.”
— Dr. Wendell Uguetto
Aside from that, people with significant health conditions, like cardiology issues, are not suitable candidates for surgery due to the added risks associated with anesthesia and the procedure itself.
Recovery After Gynecomastia Surgery
Following gynecomastia surgery, the recovery process focuses on allowing the skin to heal and adjust to its new shape. Dr. Uguetto emphasizes patience, as full recovery takes about a year.
Traditional techniques, like the Webster method, involve longer recovery times. Patients might need to avoid driving for a month, strenuous activity for two months, and may return to work within 1–2 weeks. Compared to that, Dr. Uguetto’s minimally invasive technique offers a faster recovery. Patients can potentially resume driving after 4 days and light exercise after 10 days.
Good post-operational care includes wearing compression garments, attending follow-up appointments, and maintaining scar treatment. Techniques like lymphatic drainage massage can also aid in faster healing and improved aesthetic results.
The Cost of Gynecomastia

Source: Andre Taissin from Unsplash
A regional element plays a role just as big as a surgeon’s expertise in the cost of gynecomastia surgery. Judging by Brazil, the price tag tends to be lower in the southern, northern, and northeastern regions of the country compared to major metropolitan areas like São Paulo, where surgeons have better flexibility to cater to specific audiences.
Dr. Uguetto emphasizes the variability in costs: “The cost depends on your location, the city, whether it’s a major capital, and the specific surgeon you choose. Some charge just R$8,000, while others exceed R$100,000. In my case, I charge around R$30,000 per surgery, excluding hospital fees.”
Summary
Breast enlargement in men is quite common, it is caused by hormonal imbalance and has always existed in mankind. 70% of teenagers and 30% of adult men can develop gynecomastia, regardless of their diet, age, or race.
Not so long ago, men who suddenly developed breast growth did not know what to do with it. They felt lost, unsure of which specialist to consult. But thanks to the internet, social media, and even influencers discussing the condition, more men are becoming aware that they’re not alone and can seek medical help.
This article, conducted in collaboration with Dr. Wendell Uguetto, provides a great starting point for understanding gynecomastia. We hope this article provided some helpful insights about this condition.
FAQ
👱🏼♂️ Can gynecomastia affect men’s fertility or sexual function?
Gynecomastia doesn’t directly impact fertility or sexual function, but the hormonal disbalance that causes it can.
💊 How To Get Rid of Gynecomastia?
Gynecomastia can be reduced with the help of medications, physical activity, or surgery, depending on the complexity of the case.
🤔 Is It OK To Live with Gynecomastia?
Gynecomastia is a result of hormonal imbalances, including those associated with liver diseases, as well as tumors in the kidneys and testicles. Pubertal gynecomastia is completely natural, but if it develops in adulthood, it is better to check up with a doctor.
⏳ What Happens if You Don’t Treat Gynecomastia?
In addition to possible aesthetic dissatisfaction, men with gynecomastia have an increased risk of developing breast cancer.
🔄 Will Gynecomastia Grow Back?
If the underlying hormonal issue isn’t addressed, there’s a chance gynecomastia could return. Surgery can provide long-lasting results, but it can cure hormonal issues that caused the condition.
References
1. Barros, A. C., & Sampaio, M.deC. (2012). Gynecomastia: physiopathology, evaluation and treatment. Sao Paulo medical journal = Revista paulista de medicina, 130(3), 187–197. https://doi.org/10.1590/s1516-31802012000300009
2. Braunstein G. D. (2007). Clinical practice. Gynecomastia. The New England journal of medicine, 357(12), 1229–1237. https://doi.org/10.1056/NEJMcp070677
3. Goldman R. D. (2010). Drug-induced gynecomastia in children and adolescents. Canadian family physician Medecin de famille canadien, 56(4), 344–345.
4. Nakade, D. V., Zade, M., Mehta, J., Shahane, P., & Gupta, S. (2017). Gynecomastia our surgical experience using liposuction and minimal invasive surgical excision and its psychological benefits to young patients. International Journal of Research in Medical Sciences, 5(12), 5424–5431. https://doi.org/10.18203/2320-6012.ijrms20175467
5. Niewoehner, C. B., & Schorer, A. E. (2008). Gynaecomastia and breast cancer in men. BMJ (Clinical research ed.), 336(7646), 709–713. https://doi.org/10.1136/bmj.39511.493391.BE



